Vertebroplasty is a medical procedure that involves injecting a bone cement mixture into fractured or weakened vertebrae to stabilize the spine, alleviate pain, and restore mobility for patients suffering from vertebral compression fractures. Within this guide, you will find answers to some of the more commonly asked questions regarding this spinal fracture treatment.
Is vertebroplasty a major surgery and how does it work?
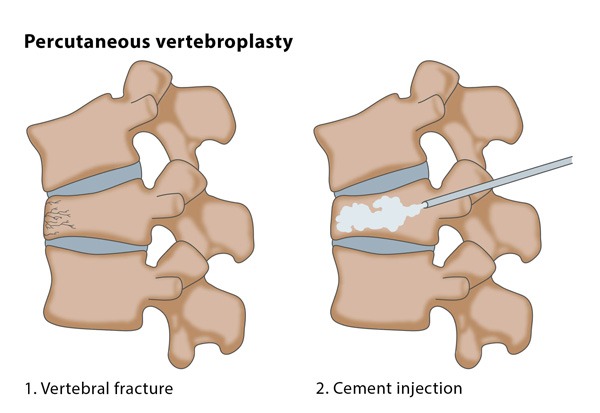
Vertebroplasty is not considered a major surgery, given its minimally invasive nature and the use of local anesthesia or conscious sedation during the procedure. This treatment involves the injection of bone cement into affected vertebrae to provide stability and pain relief, typically for patients with vertebral compression fractures. The recovery time is shorter, and the risks are generally lower than those associated with open spinal surgeries.
Vertebroplasty involves the following steps:
- Preparation: The patient is positioned face-down on the operating table. Local anesthesia or conscious sedation is administered to ensure comfort during the procedure.
- Imaging guidance: Fluoroscopy, a type of real-time X-ray imaging, is used to help the physician visualize the spine and accurately guide the needle to the target vertebra.
- Needle insertion: A small incision is made in the skin, and a hollow needle, called a trocar, is carefully inserted through the soft tissues and into the fractured or weakened vertebra.
- Cement injection: Once the needle is in place, bone cement, typically a mixture of polymethylmethacrylate (PMMA) and a contrast agent, is prepared. The cement is injected through the needle into the affected vertebra, where it quickly hardens and stabilizes the bone structure.
- Needle removal and wound closure: After the cement has hardened, the needle is removed, and the incision site is covered with a sterile dressing. Stitches are usually not required.
Is Vertebroplasty the right treatment for you?
Or Call Us at 504-732-1094
The hardened cement stabilizes the fractured vertebra, which can result in significant pain relief and improved mobility for the patient. The procedure typically takes about an hour, and patients can often return home the same day or the following day, depending on their overall health and physician recommendations.
What conditions does vertebroplasty treat?
Vertebroplasty is primarily used to treat vertebral compression fractures and provide pain relief and improved mobility. The procedure is commonly performed for patients with the following conditions:
- Osteoporosis: A progressive bone disease characterized by weakened and fragile bones, leading to an increased risk of fractures, especially in the spine.
- Spinal tumors: Both benign and malignant tumors in the spine can cause vertebral fractures or weaken the vertebral structure.
- Traumatic fractures: Vertebroplasty can be used to treat spinal compression fractures caused by trauma, such as a car accident, sports injury, or a fall, if the fracture is not excessively unstable or if other conservative treatments have failed.
- Hemangiomas: These are benign blood vessel tumors that can develop within the vertebrae and cause pain due to the pressure they exert on the surrounding bone.
It’s important to note that vertebroplasty may not be suitable for all patients with these conditions, and the decision to undergo the procedure should be made after a thorough evaluation and consultation with your doctor.
Vertebroplasty vs kyphoplasty
Vertebroplasty and kyphoplasty are both minimally invasive procedures used to treat vertebral compression fractures, primarily caused by osteoporosis, spinal tumors, or trauma. Although they share similarities, there are key differences in their techniques and objectives.
Technique:
- Vertebroplasty: In this procedure, bone cement is injected directly into the affected vertebra through a needle. The cement hardens, stabilizing the fractured vertebra and relieving pain.
- Kyphoplasty: This procedure involves two steps. First, a small balloon is inserted and inflated within the fractured vertebra to create a cavity and restore some of the lost vertebral height. The balloon is then deflated and removed, leaving the cavity in place. Next, bone cement is injected into the cavity, where it hardens to stabilize the vertebra and provide pain relief.
Objective:
- Vertebroplasty primarily focuses on stabilizing the fractured vertebra and alleviating pain. It does not aim to restore the lost vertebral height due to the fracture.
- Kyphoplasty, on the other hand, not only stabilizes the fractured vertebra but also attempts to restore the lost vertebral height by creating a cavity using the balloon. This can help improve spinal alignment and reduce the risk of future fractures.
Recovery:
Both procedures are minimally invasive and have relatively short recovery times. Patients typically return home on the same day or the following day. However, the specific recovery time and post-procedure restrictions may vary depending on the patient’s overall health and doctor’s recommendations.
Complications and risks:
Both vertebroplasty and kyphoplasty have similar risks and complications, such as infection, bleeding, nerve or spinal cord injury, and cement leakage. However, kyphoplasty generally has a lower risk of cement leakage due to the controlled filling of the cavity.
How do you prepare for vertebroplasty?
Preparing for a vertebroplasty procedure involves several steps to ensure a successful outcome and minimize risks. Here are some general guidelines to follow before undergoing vertebroplasty:
- Consultation: Discuss the procedure, its risks, and benefits with your doctor to determine if vertebroplasty is the right choice for you. Your medical history, imaging studies, and overall health will be assessed during this consultation.
- Inform your doctor: Notify your physician about any medications, supplements, or vitamins you are taking, as you may need to stop or adjust some of them before the procedure. Inform your doctor about any allergies or medical conditions, including pregnancy.
- Pre-procedure tests: Your doctor may order blood tests or other diagnostic tests to assess your overall health and suitability for the procedure.
- Fasting: You will likely be asked to avoid eating and drinking for a certain period before the procedure, typically 6-8 hours. Your doctor will provide specific instructions based on your individual case.
- Arrange transportation: Since you may be under the influence of sedation or anesthesia, arrange for someone to drive you home after the procedure.
- Follow pre-operative instructions: Your healthcare provider may give you specific instructions regarding showering, using antiseptic soap, or other measures to minimize the risk of infection.
- Wear comfortable clothing: On the day of the procedure, wear loose and comfortable clothing that is easy to remove and put on.
Keep in mind that these are general guidelines, and your doctor may give you additional or different instructions based on your specific condition and circumstances.
Are you put to sleep for vertebroplasty?
For vertebroplasty, patients are generally not put to sleep under general anesthesia. Instead, the procedure is usually performed using local anesthesia, which numbs the area where the needle is inserted, along with conscious sedation to help the patient feel relaxed and comfortable during the procedure. Conscious sedation involves administering medications that reduce anxiety and pain, allowing the patient to remain awake but in a drowsy and relaxed state.
In some cases, based on the patient’s overall health, preferences, or the complexity of the procedure, the medical team may opt for general anesthesia. However, this is less common for vertebroplasty.
What is the success rate of vertebroplasty?
The success rate of vertebroplasty varies among patients, but overall, the procedure has been found to be effective in providing pain relief and improving the quality of life for many individuals suffering from vertebral compression fractures. Studies have reported that pain relief is achieved in approximately 70-90% of patients following vertebroplasty.
It is important to note that the success rate can be influenced by various factors, including the cause of the fracture, the patient’s overall health, the experience of the medical team, and the specific technique used during the procedure. Additionally, while vertebroplasty is generally effective in providing pain relief, it may not be as effective in restoring spinal function or mobility in all cases.
As with any medical procedure, individual results may vary, and it is crucial to discuss expectations, potential outcomes, and any concerns with your doctor before undergoing vertebroplasty.
What are the risks associated with vertebroplasty?
Although vertebroplasty is a minimally invasive procedure with a relatively low risk profile, it still carries some potential risks and complications. Some of the risks associated with vertebroplasty include:
- As with any surgical procedure, there is a risk of infection at the needle insertion site or within the treated vertebra.
- There may be bleeding at the needle insertion site, although significant bleeding is rare in this procedure.
- The bone cement may leak into surrounding areas, such as the spinal canal, intervertebral disc space, or veins. In most cases, cement leakage does not cause any symptoms, but in rare instances, it can result in neurological complications, spinal cord compression, or pulmonary embolism.
- Although rare, there is a possibility of injury to the nerves or spinal cord during the procedure, which may lead to pain, numbness, or weakness.
- Vertebroplasty may increase the risk of fractures in adjacent vertebrae due to the increased stiffness of the treated vertebra and the altered load distribution along the spine.
- There are potential risks with any procedure involving anesthesia, including allergic reactions and respiratory issues, although these are more commonly associated with general anesthesia rather than local anesthesia or conscious sedation.
- Some patients may not experience significant pain relief following the procedure, or the pain relief may be temporary.
Is vertebroplasty safe for elderly?
Vertebroplasty is generally considered safe for elderly patients, as it is a minimally invasive procedure with relatively low risks and complications compared to more invasive spinal surgeries. In fact, many elderly patients suffer from vertebral compression fractures due to age-related conditions like osteoporosis, making vertebroplasty a commonly performed procedure in this population.
The procedure can help alleviate pain, stabilize the spine, and improve mobility for elderly patients, contributing to a better quality of life. However, it is important to consider each patient’s overall health, medical history, and the severity of their condition when determining the appropriateness of vertebroplasty.
Elderly patients may have an increased risk of complications due to factors such as reduced bone quality, pre-existing medical conditions, or a weakened immune system. Therefore, a thorough evaluation and consultation with a qualified healthcare provider are essential before deciding to undergo vertebroplasty.
Who is a good candidate for vertebroplasty?
A good candidate for vertebroplasty is typically someone who has a vertebral compression fracture that has not responded well to conservative treatments and is experiencing significant pain, reduced mobility, or decreased quality of life. Some factors that may make a person a suitable candidate for vertebroplasty include:
- Vertebral compression fracture caused by osteoporosis, trauma, or spinal tumors.
- Persistent and debilitating pain that has not improved with conservative treatments such as pain medication, physical therapy, or wearing a back brace.
- Recent fracture: Vertebroplasty is generally more effective when performed within a few weeks to a few months after the fracture occurs.
- Fracture location: Vertebroplasty is most suitable for treating fractures in the thoracic and lumbar regions of the spine.
- Overall health: Good candidates should be in reasonably good health to tolerate the procedure and minimize the risk of complications.
It’s important to note that vertebroplasty may not be suitable for everyone, even if they meet some of the criteria mentioned above. Patients with certain medical conditions, very old fractures, or fractures causing spinal instability or significant spinal canal narrowing may not be ideal candidates for vertebroplasty.
Unsure if you’re a candidate for Vertebroplasty?
How long does it take to recover from vertebroplasty?
Recovery time from vertebroplasty can vary from patient to patient, depending on their overall health and the specifics of their condition. However, in general, patients can expect a relatively quick recovery due to the minimally invasive nature of the procedure.
Most patients experience pain relief immediately or within a few days following vertebroplasty. They are typically able to return home on the same day or the day after the procedure. Some patients may be advised to avoid strenuous activities, heavy lifting, or excessive bending or twisting for a short period, usually a few days to a few weeks, as a precautionary measure.
Patients are usually encouraged to gradually resume their normal daily activities and may benefit from participating in a physical therapy program to help strengthen their back muscles, improve flexibility, and promote overall spinal health.
It is important to follow the specific post-procedure instructions provided by your doctor to ensure a successful recovery. As with any medical procedure, individual recovery times may vary. It is crucial to consult with your doctor to discuss expectations and any concerns related to the recovery process.
Contact the experts at Lonseth today to learn more about vertebroplasty and to determine if it’s the appropriate procedure for you.
